KEY TAKEAWAYS
- Medicare Advantage represents a rare opportunity for both membership growth and massive value creation.
- The days of simple “me, too” product offerings that lack purpose-built capabilities may be ending soon.
- Models bringing about tighter payer and provider collaboration have shown superior results, and are in the stages of early proliferation.
By the time you finish reading this article, another 30 Baby Boomers will have turned 65 years old, aging in to Medicare. The “Silver Tsunami” is upon us. But don’t try to put all Boomers in a one-size-fits-all box. Boomers currently range from 55 to 75 years old and are a more diverse generation in terms of their experiences, expectations, and attitudes – particularly when it comes to matters of health. Plus, they’re the first generation to enter their Medicare years equipped with technology, tools, and information regarding their health and care options. They bring their experiences of having cared for the prior generation (some, in fact, are still caring for their parents).
However, Boomers also bring with them healthcare needs that are perhaps higher relative to past generations’ needs. They’re more likely to deal with obesity, and sixty percent of Boomers have already been diagnosed with more than one chronic condition like arthritis, diabetes, heart disease, or osteoporosis. And, they’re already on more medications and require more dietary interventions than past generations – adding operational and financial stress to the US healthcare system.
Seeking beacons of hope, Medicare Advantage plans stand apart as a path to align this growing senior population with a reconstituted healthcare ecosystem. While there are proven models in operation nationwide, they still only reach a fraction of this market. Therefore, it will be critical that health plans, providers, and innovators continue to push the envelope if they are to meet the expanded demands of this new generation of seniors and their more complex medical needs.
There’s an incredible opportunity to dramatically impact the future of this generation, but it rests on the notion of collapsing older, siloed models.
MEDICARE ADVANTAGE’S RECENT STRATEGIC MAKEOVER
With 10,000 new Medicare-eligible beneficiaries per day – nearly 3.5 million per year – Medicare Advantage represents a very rare opportunity for new membership growth. Adoption of Medicare Advantage plans by seniors has picked up considerably in the past decade, growing from 24 percent of the Medicare-eligible population in 2010 to 34 percent in 2019. With spending hovering somewhere near $10,000 per member per year, and payments on the rise (3.4 percent for 2019 and 2.5 percent for 2020), the rush is on to build products and solutions for this segment. (And, this is to say nothing of the possibilities that might arise from more accurate risk coding and improved Medicare Advantage Star performance.)
Yet, historically, Medicare Advantage strategies have not sought to fundamentally transform care or create differentiated, senior-focused networks and care models. Instead, most plans sought success by making small changes to underlying benefits and provider incentives and applying other managed care tools. However, as payers and providers have realized Medicare Advantage’s growth, profit, and mission-fulfilling potential, competition has greatly intensified. This all suggests the days of simple “me, too” product offerings that lack purpose-built capabilities may soon be ending soon.
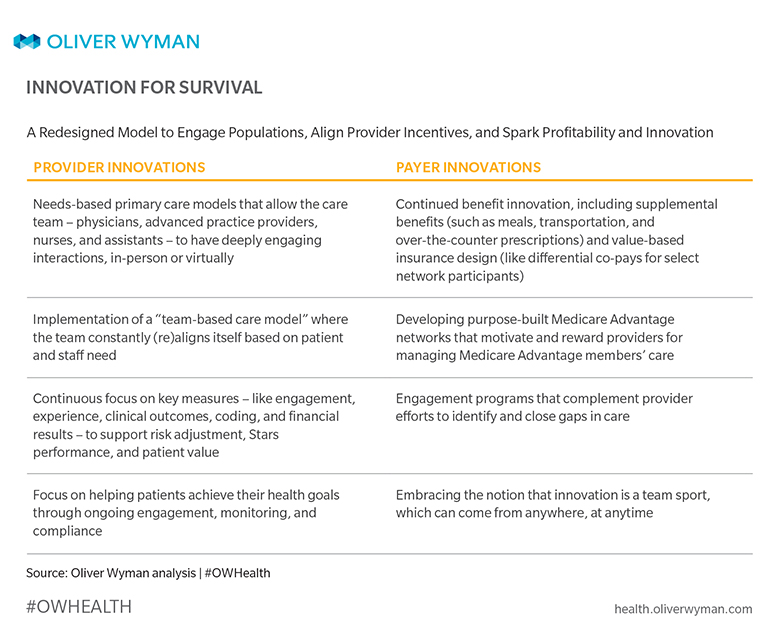
Fast-forward to now when we see many examples of payers and providers driving innovation in different geographic markets nationwide, with specific and very intentional strategies focused on winning the Medicare Advantage gold rush. Recognizing both the clinical and administrative complexities of serving this population, payers and providers are more frequently collaborating more to align incentives and deploy purpose-built care models.
Two prominent approaches are bringing this innovation to local markets:
- Plan-led. A networked health plan has created aligned incentives with its provider partners to drive much improved clinical management. The plan is aligning its network towards high- performing provider partners who have incentives tied to member success measures (like quality, outcomes, and cost). This model is founded upon integrated delivery systems that have deployed patient-centered medical homes, along with other provider partnerships that innovate through risk-based payment arrangements and customized product sets.
- Provider-led. There’s a growing number of provider-led Medicare Advantage solutions where providers integrate tightly with health plans (or build their own), and then build focused care models to envelope the full patient journey – from needs identification to holistic management, thus sparking higher patient engagement levels. These plans are driving higher Star ratings, more patient satisfaction, and increased professional satisfaction for providers.
Inherent to all Medicare Advantage models is an intense focus on data, analytics, and technology that (1) creates greater insights around where and how to support members/patients on their journey; and (2) enables clarity as to who will engage these patients at varying points along that journey. Data and insights are only valuable when closely tethered to an integrated team and population-focused care model.
EXHIBIT 1
HOW PAYERS AND PROVIDERS WILL EMERGE VICTORIOUS
Looking ahead, winning in the Medicare Advantage marketplace will require payers and providers to collaborate more closely on strategies, and then closely integrate operations and support models across the member/patient journey. Both are a departure from the norm. Rendering holistic, proactive care doesn’t easily fit inside a traditional fee-for-service model. Enabling proactive intervention requires data and analytics that many payers either don’t possess or haven’t traditionally shared with their provider partners. The resulting models will be far more impactful and will eliminate many of consumers' current hassles. This will be a welcome departure from the status quo. And those payers and providers that drive these innovations stand to create immense value – not just for the health ecosystem, but for the communities they serve. Tomorrow's winners will emerge victorious from models wherein benefits and care delivery become a singular idea focused on consumer value.
For more Oliver Wyman Health insights, visit health.oliverwyman.com.
ABOUT THE AUTHORS
- Melinda Durr, Partner, Health & Life Sciences, Oliver Wyman
- Dan Shellenbarger, Partner, Health & Life Sciences, Oliver Wyman
- Deblina Ghosh, Principal, Health & Life Sciences, Oliver Wyman



