Editor's Note: For more information about this survey, see "Insurers to Expand Presence in Affordable Care Act Marketplaces Despite Uncertainty" in the Wall Street Journal.
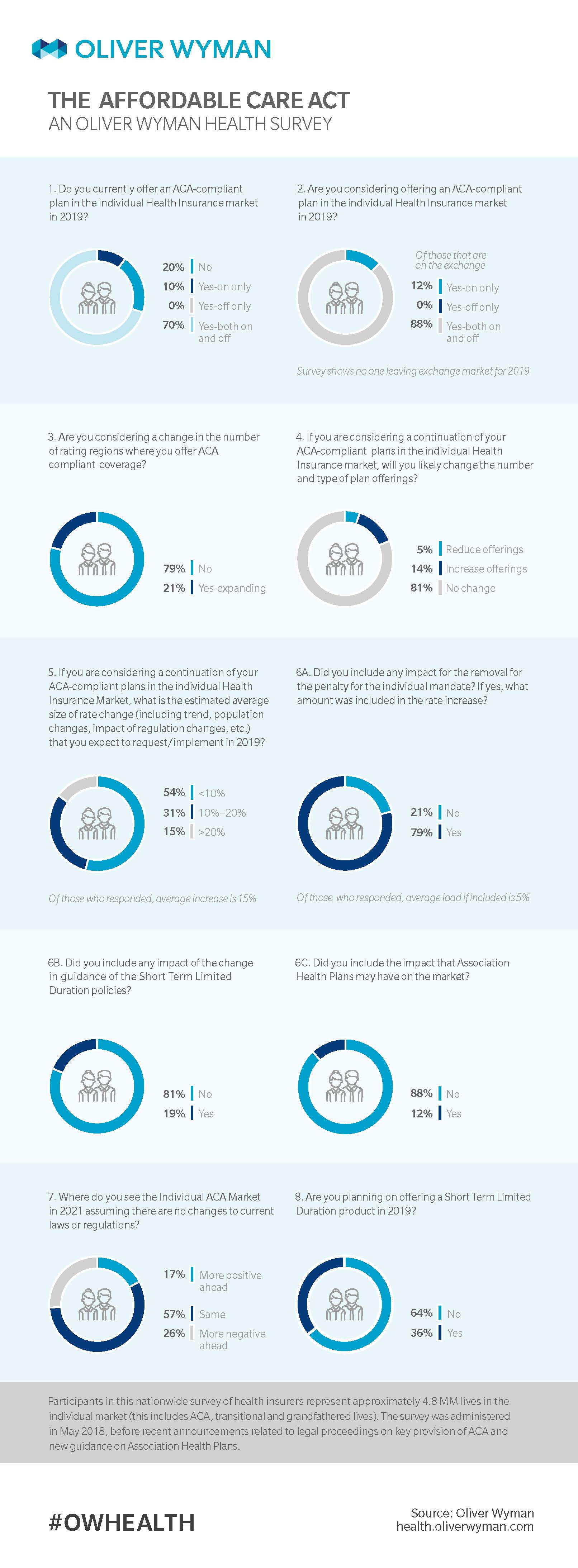
One year ago, we conducted a nationwide Oliver Wyman Actuarial Consulting survey to better understand the market impact of uncertainty related to Cost Sharing Reduction (CSR) funding and other policy considerations. Here, in an updated version of this annual survey, we conclude based on feedback from 30 respondents – 24 of whom are in the market, and none of which solely participate in the off-Exchange market – that there is indeed greater market stabilization as premiums have largely “absorbed” the impact of both risk and policy announcements. That said, premium increases are still meaningfully above medical trend reflecting that adjustments to key provisions of the Affordable Care Act (ACA) are still affecting rates.
Following the Trump administration’s end to cost sharing reduction CSR payments late last year, and recent news from the Department of Justice that the ACA's individual mandate is unconstitutional, we’ve determined in our updated survey that the health market has remained on even keel. Of emphasis is that the weighted average rate increases for 2017 was 22 percent, as per the Department of Health and Human Services. But this year’s expected average rate increase fell to a reported average of 15 percent. Just over half of respondents confirmed that if they were considering continuing their ACA-compliant plans in the Individual Health Insurance Market, their estimated average size of rate change – including factors such as trend, population changes, and the impact of regulation changes – increased by no more than 10 percent, with nearly 1 in 3 noting an increase between 10 – 20 percent.
Here is a summary of four key updated findings:
1. Carrier Participation in an ACA-Compliant Market is Steady
Updated Oliver Wyman Actuarial Consulting analysis from the year prior confirms the number of carriers participating in the ACA-compliant market appears to have flattened off. Twenty one percent did respond however that they plan to expand geographically and 14 percent plan to increase their offerings. That said, most surveyed carriers – 57 percent – envision the 2021 market to look similar to the market of today. However, the remaining individuals surveyed say the future market will not be an improvement compared to the market of today, with 1 in 4 expecting more negative changes to the Individual ACA Market in 2021 (assuming there are no changes to current laws or regulations), and 17 percent anticipating market improvement over the next three years.
2. Rate Increases Top Medical Trends
According to our new survey findings, rate increases are still higher than medical trends, with a total average increase of 15 percent. This number is likely due to factors such as widespread hesitation and uncertainty following deletion of the ACA’s individual mandate. Results show potential changes in the ACA rules for there was minimal market impact on premiums in terms of short term limited-duration insurance plans (STLDIs) and association health plans (AHPs) had minimal impact on the market premiums. However, we did not ask respondents if state regulators were implementing rules or regulations that limited the impact of STLDIs or AHPs.
3. Most Carriers Incorporated Individual Mandate Changes
This year’s survey results conclude that respondents believe the removal of the individual mandate impacted market premiums between 1 to 10 percent, with an average load of 5 percent included in the rates. (We acknowledge answers may have been different, however, had we conducted this survey prior to the aforementioned Department of Justice announcements.)
Seventy-nine percent of respondents said they included any impact for removal of the individual mandate penalty.
4. But Few Incorporated Short Term Duration Policy Updates
While the majority of those surveyed said they did not integrate short term duration policies into their plan operations, most respondents – 81 percent – said they were investigating offering a short-term, limited duration insurance (STDLI) plan, such as launching an innovative product or implementing a change to a currently available product. Over 1 in 3 surveyed said they plan to offer this product next year.